Risk of cancer with gastric symptoms in primary care;
http://www.nature.com/bjc/journal/v108/n1/full/bjc2012551a.html
The important bit is this table. Look at the PPVs (positive predictive values) on the right hand side. 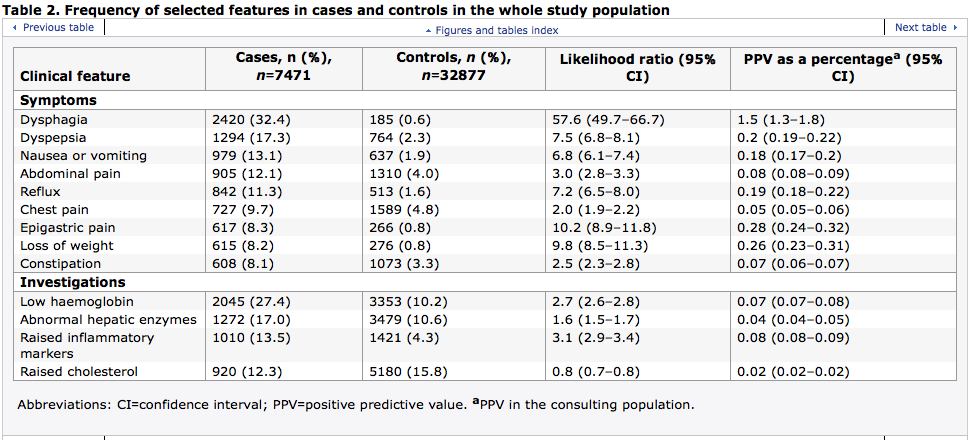
so ‘dyspepsia’ in this population signals cancer 0.2% of the time.
Other studies put it a bit higher, but I think this is the most relevant UK data (you have to go through the paper to get the full workings.)
Early diagnosis projects are also trying to find what symptoms are best predictors for cancer.
 http://www.macmillan.org.uk/Documents/AboutUs/Health_professionals/EarlyDiagnosis/QCancerOvarian.pdf
http://www.macmillan.org.uk/Documents/AboutUs/Health_professionals/EarlyDiagnosis/QCancerOvarian.pdf
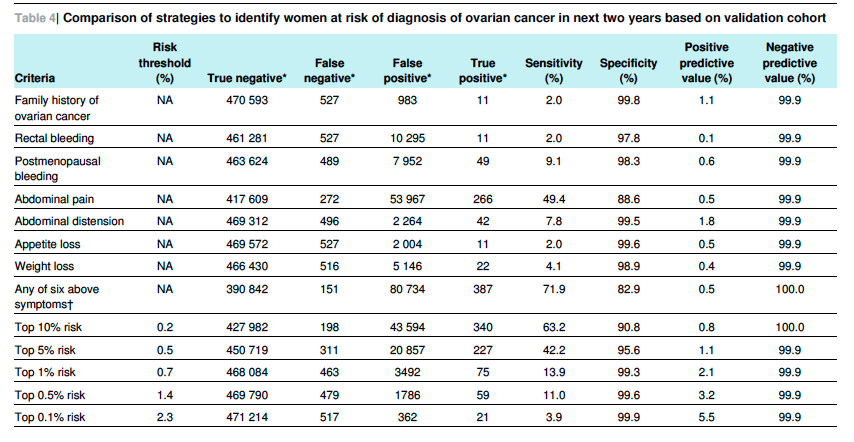
Essentially, women that you work out as being in the top 10% band for risk of having ovarian cancer turn out to have a 0.8% chance of having it.
Essentially GPs have to decide whether to refer someone under a 2week wait (suspected cancer) or 18 week appointment – my concern has always been that we simply can’t safely do this. See this paper – about 18% of 2 week referred patients end up with a diagnosis of cancer. But almost 10% of the patients referred outwith guidelines but under a 2 week wait request (which could have been rejected) ended up with a diagnosis of cancer. In other words – urgent referral criteria aren’t very good.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3207087/
PATIENT SURVEYS
British Social Attitudes survey
http://www.natcen.ac.uk/our-research/research/british-social-attitudes/
http://www.kingsfund.org.uk/projects/bsa-survey-2014%20
Friends and family
http://www.england.nhs.uk/statistics/statistical-work-areas/friends-and-family-test/
Click to access Patient-FFT-Stats-Commentary-December-2014.pdf
Ipsos MORI
http://www.england.nhs.uk/statistics/2014/07/03/gp-patient-survey-2013-14/
Scotland equivalent

Comments are closed.